Coronavirus
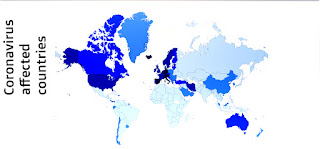 |
| Coronavirus Map |
Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) is the name given to the 2019 novel coronavirus. COVID-19 is the name given to the disease associated with the virus. SARS-CoV-2 is a new strain of coronavirus that has not been previously identified in humans
Coronaviruses are a large family of viruses which may cause illness in animals or humans. In humans, several coronaviruses are known to cause respiratory infections ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS). The most recently discovered coronavirus causes coronavirus disease COVID-19.
Coronaviruses are a large family of viruses which may cause illness in animals or humans. In humans, several coronaviruses are known to cause respiratory infections ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS). The most recently discovered coronavirus causes coronavirus disease COVID-19.
Q. Where do coronaviruses come from ?
Coronaviruses are viruses that circulate among animals with some of them also known to infect humans.
Bats are considered natural hosts of these viruses yet several other species of animals are also known to act as sources. For instance, Middle East Respiratory Syndrome Coronavirus (MERS-CoV) is transmitted to humans from camels, and Severe Acute Respiratory Syndrome Coronavirus-1 (SARS-CoV-1) is transmitted to humans from civet cats.
Q. Is this virus comparable to SARS or to the seasonal flu ?
The novel coronavirus detected in China in 2019 is closely related genetically to the SARS-CoV-1 virus. SARS emerged at the end of 2002 in China, and it caused more than 8 000 cases in 33 countries over a period of eight months. Around one in ten of the people who developed SARS died.
As of 30 March 2020, the COVID-19 outbreak had caused over 700 000 cases worldwide since the first case was reported in China in January 2020. Of these, more than 30 000 are known to have died.
While the viruses that cause both COVID-19 and seasonal influenza are transmitted from person-to-person and may cause similar symptoms, the two viruses are very different and do not behave in the same way.
ECDC estimates that between 15 000 and 75 000 people die prematurely due to causes associated with seasonal influenza infection each year in the EU, the UK, Norway, Iceland and Liechtenstein. This is approximately 1 in every 1 000 people who are infected. Despite the relatively low mortality rate for seasonal influenza, many people die from the disease due to the large number of people who contract it each year. The concern about COVID-19 is that, unlike influenza, there is no vaccine and no specific treatment for the disease. It also appears to be more transmissible than seasonal influenza. As it is a new virus, nobody has prior immunity, which means that the entire human population is potentially susceptible to SARS-CoV-2 infection
Coronaviruses are viruses that circulate among animals with some of them also known to infect humans.
Bats are considered natural hosts of these viruses yet several other species of animals are also known to act as sources. For instance, Middle East Respiratory Syndrome Coronavirus (MERS-CoV) is transmitted to humans from camels, and Severe Acute Respiratory Syndrome Coronavirus-1 (SARS-CoV-1) is transmitted to humans from civet cats.
Q. Is this virus comparable to SARS or to the seasonal flu ?
The novel coronavirus detected in China in 2019 is closely related genetically to the SARS-CoV-1 virus. SARS emerged at the end of 2002 in China, and it caused more than 8 000 cases in 33 countries over a period of eight months. Around one in ten of the people who developed SARS died.
As of 30 March 2020, the COVID-19 outbreak had caused over 700 000 cases worldwide since the first case was reported in China in January 2020. Of these, more than 30 000 are known to have died.
While the viruses that cause both COVID-19 and seasonal influenza are transmitted from person-to-person and may cause similar symptoms, the two viruses are very different and do not behave in the same way.
ECDC estimates that between 15 000 and 75 000 people die prematurely due to causes associated with seasonal influenza infection each year in the EU, the UK, Norway, Iceland and Liechtenstein. This is approximately 1 in every 1 000 people who are infected. Despite the relatively low mortality rate for seasonal influenza, many people die from the disease due to the large number of people who contract it each year. The concern about COVID-19 is that, unlike influenza, there is no vaccine and no specific treatment for the disease. It also appears to be more transmissible than seasonal influenza. As it is a new virus, nobody has prior immunity, which means that the entire human population is potentially susceptible to SARS-CoV-2 infection
Q. What is the mode of transmission? How (easily) does it spread ?
While animals are believed to be the original source, the virus spread is now from person to person (human-to-human transmission). There is not enough epidemiological information at this time to determine how easily this virus spreads between people, but it is currently estimated that, on average, one infected person will infect between two and three other people.
The virus seems to be transmitted mainly via small respiratory droplets through sneezing, coughing, or when people interact with each other for some time in close proximity (usually less than one metre). These droplets can then be inhaled, or they can land on surfaces that others may come into contact with, who can then get infected when they touch their nose, mouth or eyes. The virus can survive on different surfaces from several hours (copper, cardboard) up to a few days (plastic and stainless steel). However, the amount of viable virus declines over time and may not always be present in sufficient numbers to cause infection.
The incubation period for COVID-19 (i.e. the time between exposure to the virus and onset of symptoms) is currently estimated to bet between one and 14 days.
We know that the virus can be transmitted when people who are infected show symptoms such as coughing. There is also some evidence suggesting that transmission can occur from a person that is infected even two days before showing symptoms; however, uncertainties remain about the effect of transmission by non-symptomatic persons.
While animals are believed to be the original source, the virus spread is now from person to person (human-to-human transmission). There is not enough epidemiological information at this time to determine how easily this virus spreads between people, but it is currently estimated that, on average, one infected person will infect between two and three other people.
The virus seems to be transmitted mainly via small respiratory droplets through sneezing, coughing, or when people interact with each other for some time in close proximity (usually less than one metre). These droplets can then be inhaled, or they can land on surfaces that others may come into contact with, who can then get infected when they touch their nose, mouth or eyes. The virus can survive on different surfaces from several hours (copper, cardboard) up to a few days (plastic and stainless steel). However, the amount of viable virus declines over time and may not always be present in sufficient numbers to cause infection.
The incubation period for COVID-19 (i.e. the time between exposure to the virus and onset of symptoms) is currently estimated to bet between one and 14 days.
We know that the virus can be transmitted when people who are infected show symptoms such as coughing. There is also some evidence suggesting that transmission can occur from a person that is infected even two days before showing symptoms; however, uncertainties remain about the effect of transmission by non-symptomatic persons.
Q. When is a person infectious ?
The infectious period may begin one to two days before symptoms appear, but people are likely most infectious during the symptomatic period, even if symptoms are mild and very non-specific. The infectious period is now estimated to last for 7-12 days in moderate cases and up to two weeks on average in severe cases
Medical information
Q. What are the symptoms of COVID-19 infection ?
Symptoms of COVID-19 vary in severity from having no symptoms at all (being asymptomatic) to having fever, cough, sore throat, general weakness and fatigue and muscular pain and in the most severe cases, severe pneumonia, acute respiratory distress syndrome, sepsis and septic shock, all potentially leading to death. Reports show that clinical deterioration can occur rapidly, often during the second week of disease.
Recently, anosmia – loss of the sense of smell – (and in some cases the loss of the sense of taste) have been reported as a symptom of a COVID-19 infection. There is already evidence from South Korea, China and Italy that patients with confirmed SARS-CoV-2 infection have developed anosmia/hyposmia, in some cases in the absence of any other symptoms.
Q. Are some people more at risk than others ?
Elderly people above 70 years of age and those with underlying health conditions (e.g. hypertension, diabetes, cardiovascular disease, chronic respiratory disease and cancer) are considered to be more at risk of developing severe symptoms. Men in these groups also appear to be at a slightly higher risk than females
Q. Are children also at risk of infection and what is their potential role in transmission ?
Children make up a very small proportion of reported COVID-19 cases, with about 1% of all cases reported being under 10 years, and 4% aged 10-19 years. Children appear as likely to be infected as adults, but they have a much lower risk than adults of developing symptoms or severe disease. There is still some uncertainty about the extent to which asymptomatic or mildly symptomatic children transmit disease.
Q. Is there a treatment for the COVID-19 disease ?
There is no specific treatment or vaccine for this disease.
Healthcare providers are mostly using a symptomatic approach, meaning they treat the symptoms rather than target the virus, and provide supportive care (e.g. oxygen therapy, fluid management) for infected persons, which can be highly effective.
In severe and critically ill patients, a number of drugs are being tried to target the virus, but the use of these need to be more carefully assessed in randomised controlled trials. Several clinical trials are ongoing to assess their effectiveness but results are not yet available.
As this is a new virus, no vaccine is currently available. Although work on a vaccine has already started by several research groups and pharmaceutical companies worldwide, it may be months to more than a year before a vaccine has been tested and is ready for use in humans.
Q. When should I be tested for COVID-19 ?
Current advice for testing depends on the stage of the outbreak in the country or area where you live. Testing approaches will be adapted to the situation at national and local level. National authorities may decide to test only subgroups of suspected cases based on the national capacity to test, the availability of necessary equipment for testing, the level of community transmission of COVID-19, or other criteria
Point's
hospitalised patients with severe respiratory infections;
symptomatic healthcare staff including those with mild symptoms;
cases with acute respiratory infections in hospital or long-term care facilities;
patients with acute respiratory infections or influenza-like illness in certain outpatient clinics or hospitals;
elderly people with underlying chronic medical conditions such as lung disease, cancer, heart failure, cerebrovascular disease, renal disease, liver disease, diabetes, and immunocompromising conditions.
Q. Where can I get tested ?
If you are feeling ill with COVID-19 symptoms (such as fever, cough, difficulty breathing, muscle pain or general weakness), it is recommended that you contact your local healthcare services online or by telephone. If your healthcare provider believes there is a need for a laboratory test for the virus that causes COVID-19, he/she will inform you of the procedure to follow and advise where and how the test can be performed.
Q. How can we differentiate between hay fever/pollen allergy related respiratory symptoms and COVID-19 infection ?
Someone with COVID-19 usually has mild, flu-like symptoms (see above question 1), which are rather common and need to be distinguished from similar symptoms caused by common cold viruses and from allergic symptoms during springtime.
The following table presents a comparison of the most common symptoms of all three conditions according to their reported frequency.
It is good to bear in mind that the definitive diagnosis of COVID-19 is not clinical, but through laboratory testing of a sample from the nose or mouth.
Prevention
Q. How can I avoid getting infected ?
The virus enters your body via your eyes, nose and/or mouth, so it is important to avoid touching your face with unwashed hands.
Washing of hands with soap and water for at least 20 seconds, or cleaning hands thoroughly with alcohol-based solutions, gels or tissues is recommended in all settings. It is also recommended to stay one metre or more away from people infected with COVID-19 who are showing symptoms, to reduce the risk of infection through respiratory droplets.
Q. How can I avoid infecting others ?
Cough or sneeze into your elbow or use a tissue. If you use a tissue, dispose of it carefully after a single use.
Wash your hands with soap and water for at least 20 seconds.
Stay one metre or more away from people to reduce the risk of spreading the virus through respiratory droplets.
If you feel unwell, stay at home. If you develop any symptoms suggestive of COVID-19, you should immediately call your healthcare provider for advice.
Q. What is physical distancing and why and how should I do it ?
Physical distancing aims to reduce physical contact between potentially infected people and healthy people, or between population groups with high rates of transmission and others with low or no level of transmission. The objective of this is to decrease or interrupt the spread of COVID-19.
Note that the term ‘physical distancing’ means the same thing as the widely used term ‘social distancing’, but it more accurately describes what is intended, namely that people keep physically apart. Physical distancing measures might be implemented over an extended period and their success depends on ensuring that people maintain social contact – from a distance – with friends, family and colleagues. Internet-based communications and the phone are therefore key tools for ensuring a successful physical distancing strategy.
On a personal level, you can perform physical distancing measures by:
Voluntarily self-isolating if you know you have the virus that causes COVID-19, or if you have suggestive respiratory symptoms, or if you belong to a high-risk group (i.e. you are aged 70 years or more, or you have an underlying health condition).
Point's
The full or partial closure of educational institutions and workplaces;
Limiting the number of visitors and limiting the contact between the residents of confined settings, such as long-term care facilities and prisons;
Cancellation, prohibition and restriction of mass gatherings and smaller meetings;
Mandatory quarantine of buildings or residential areas;
Internal or external border closures;
Stay-at-home restrictions for entire regions or countries.
Q. What should I do if I develop symptoms of COVID-19 ?
Follow the guidelines of the public health authorities in your area on the steps to take or call the local COVID-19 helpline.
Q. Are face masks effective in protecting against COVID-19 ?
If you are infected, the use of surgical face masks may reduce the risk of you infecting other people. On the other hand there is no evidence that face masks will effectively prevent you from becoming infected with the virus. In fact, it is possible that the use of face masks may even increase the risk of infection due to a false sense of security and increased contact between hands, mouth and eyes while wearing them. The inappropriate use of masks also may increase the risk of infection.
Q. Is there a vaccine against the virus ?
There are currently no vaccines against human coronaviruses, including the virus that causes COVID-19. This is why it is very important to prevent infection and to take measures to contain further spread of the virus.
Q. How long will it take to develop a vaccine ?
The development of vaccines take time. Several pharmaceutical companies and research laboratories are working on vaccine candidates. It will, however, take months or years before any vaccine can be widely used, as it needs to undergo extensive testing in clinical trials to determine its safety and efficacy. These clinical trials are an essential precursor to regulatory approval and usually take place in three phases. The first, involving a few dozen healthy volunteers, tests the vaccine for safety, monitoring for adverse effects. The second, involving several hundred people, usually in a part of the world badly affected by the disease, looks at how effective the vaccine is in the field, and the third does the same in several thousand people.
Q. Am I protected against COVID-19 if I had the influenza vaccine this year ?
Influenza and the virus that causes COVID-19 are two very different viruses and the seasonal influenza vaccine will not protect against COVID-19.
Watch The Video To Know More:-
video
No comments:
Post a Comment